| How do I Find a Syringe Service Program to Collaborate With? |
| While the number of SSPs continue to grow in NC there are only 48 programs in existence serving 59 out of the 100 counties in our state. To find out if an SSP is operational in your local area see the NCDHHS website for the most complete up-to-date listings |
| Syringe Service Programs in North Carolina |
| If you fail to see an SSP operational in your existing county, don’t let that stop you from seeking collaboration with SSP’s in adjacent counties. Many areas, especially rural communities, where the opioid burden is often the greatest, have no harm reduction services. As extension sites to existing SSPs, Community Pharmacies can play a crucial role in bringing services to a community in need, especially in desert areas |
OK, I've Identified a Syringe Service Program in my Surrounding Area.
NOW WHAT? |
| Reach out to the contact person for the SSP found in the NCDHHS list above and let them know of your interest in a potential collaboration. |
| Check the SSP's hours of operation. Pharmacies partnering with SSPs that operate on reduced hours provide added value due to a pharmacy's extended hours of operation |
| What Things Should we Consider in Developing a Partnership? |
| Consider Visiting the SSP |
Shadow those employees who work closely with clients. Learn how they engage their clients and, if possible, see if you can take part in a visit from intake to completion.
Pharmacies partnering with SSPs in a 2021 NCAP Pilot initiative cited this activity as one of the most helpful in understanding the ethical and professional obligations they as healthcare providers have in educating and guiding people who inject drugs (PWID) toward safe practices.
|
| Learn What Injection Supplies are Commonly Given to SSP Clients |
This is eye-opening for many pharmacists. As healthcare providers, pharmacists may find it difficult to adjust to providing items viewed as drug paraphernalia; however, it's essential to understand why exchanging these items is so important.
Lessons learned from NCAP’s Pilot found that SSPs packaged their injection supplies in such an organized fashion that it was easier for both pharmacies and SSPs to simply agree to provide the same package for ease of distribution and collection of returns. |
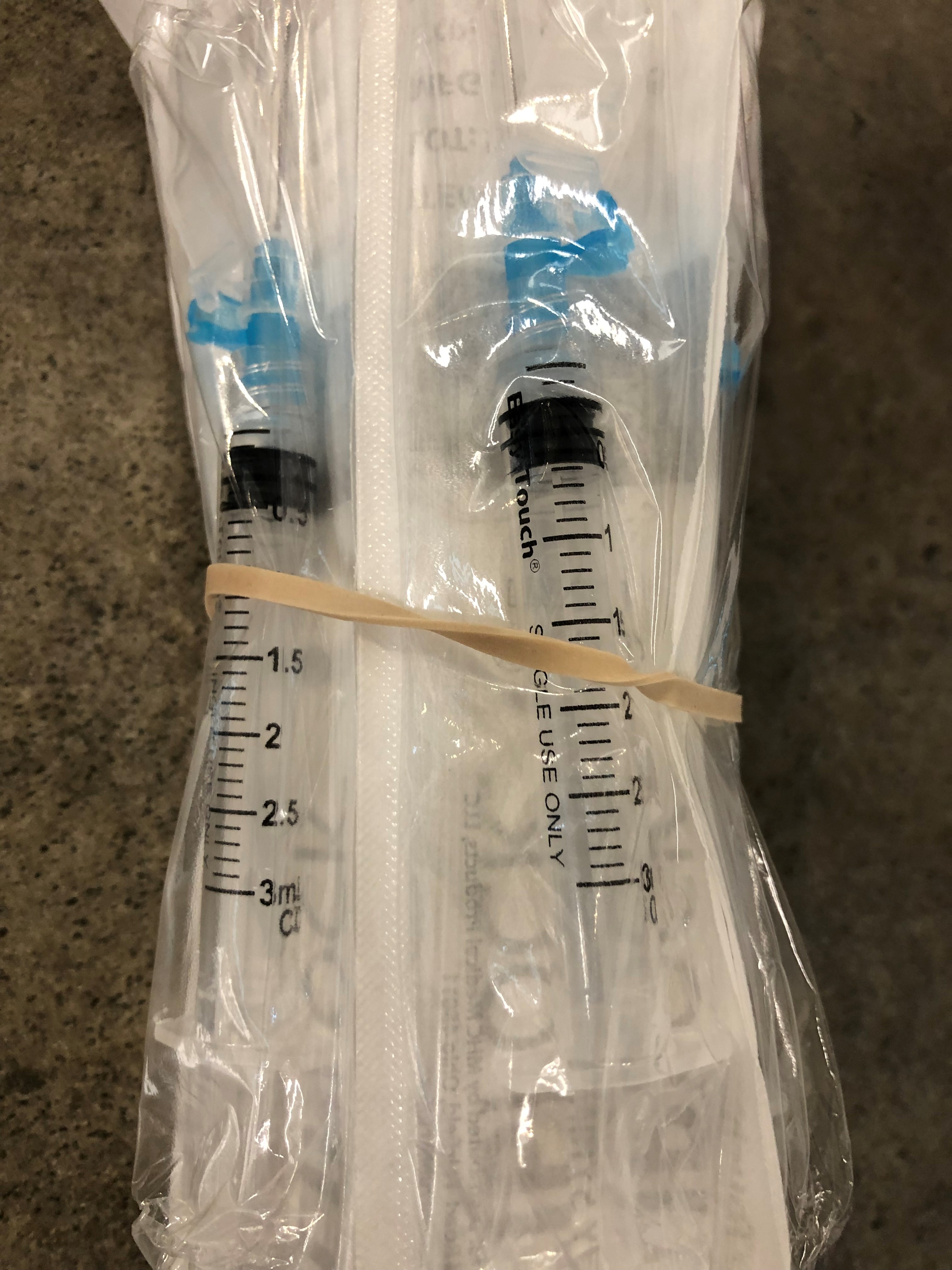 
Syringes, Needles, and Sharps Containers |
Sharing and reusing needles is a common practice among PWID and leads to an increased risk of infection and disease transmission. Repeated use of needles results in such profound structural changes to the needle itself that these changes alone create a breeding ground for bacteria and blood-borne contamination. |
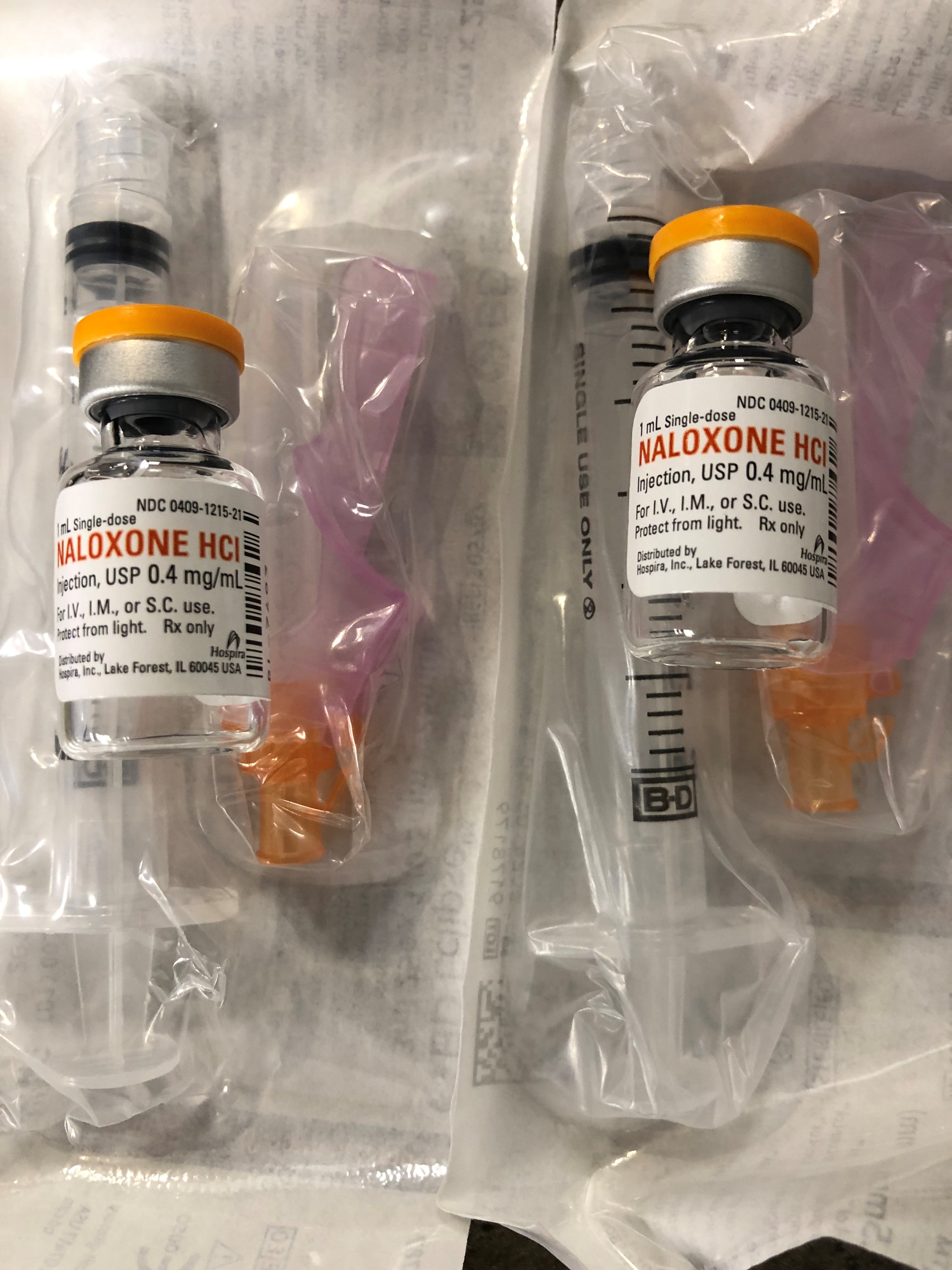
Naloxone Kits |
PWID are at high risk for drug overdose. Naloxone is a low-risk, easy-to-use life-saving antidote to overdose from heroin and other opioids. It can reduce opioid overdose deaths by as much as 50% when combined with proper training and distribution. |
Wound Care
(Alcohol Wipes, Bandages, Gauze, Antibiotic Ointment) |
Access to general wound care is essential to preventing the development and spread of infection |
Safe Use Supplies
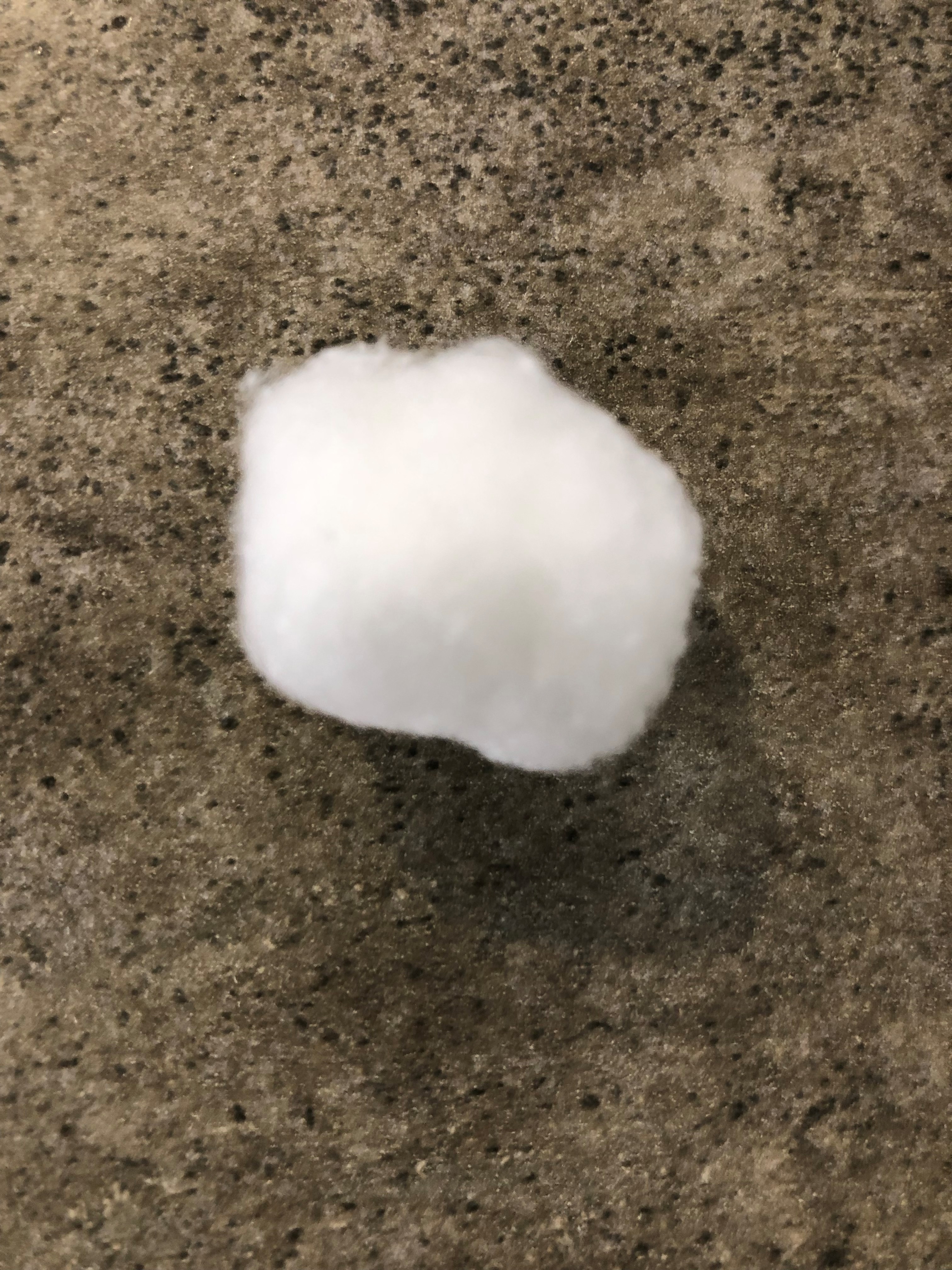
(Tourniquets, Cookers, Cotton Swabs, Sterile Water) |
When PWID prepare and inject substances, the supplies used may come into contact with blood that can spread HIV or hepatitis B, or C. To prevent the spread of infection, SSPs provide these supplies so clients will have new (unused) equipment for every injecting event. |
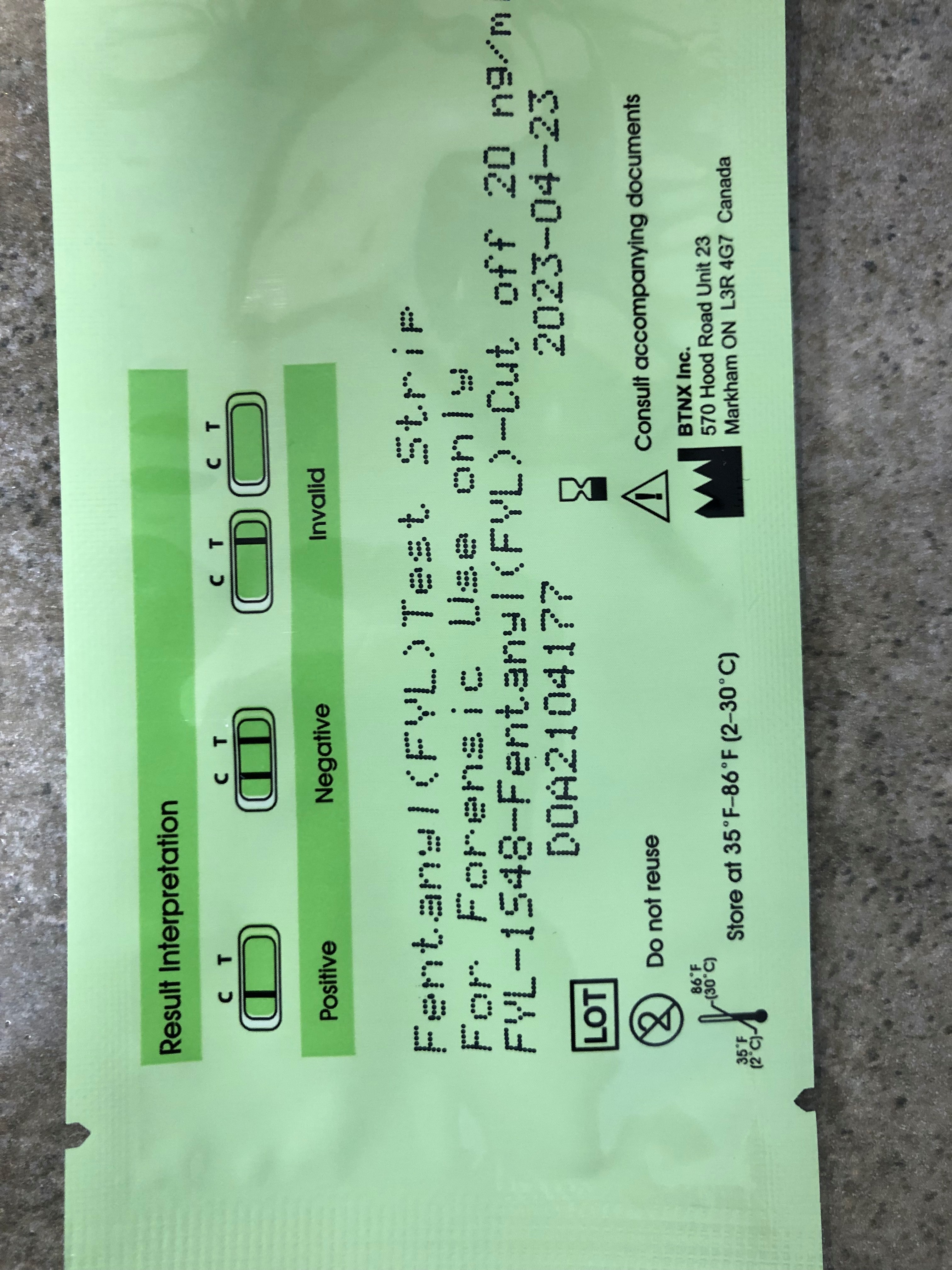
Fentanyl Test Strips |
Fentanyl Test Strips allow PWID to be more informed about the drugs they are buying and using, leading to behavior change and the adoption of increased harm reduction measures, including sharing information among peers. |
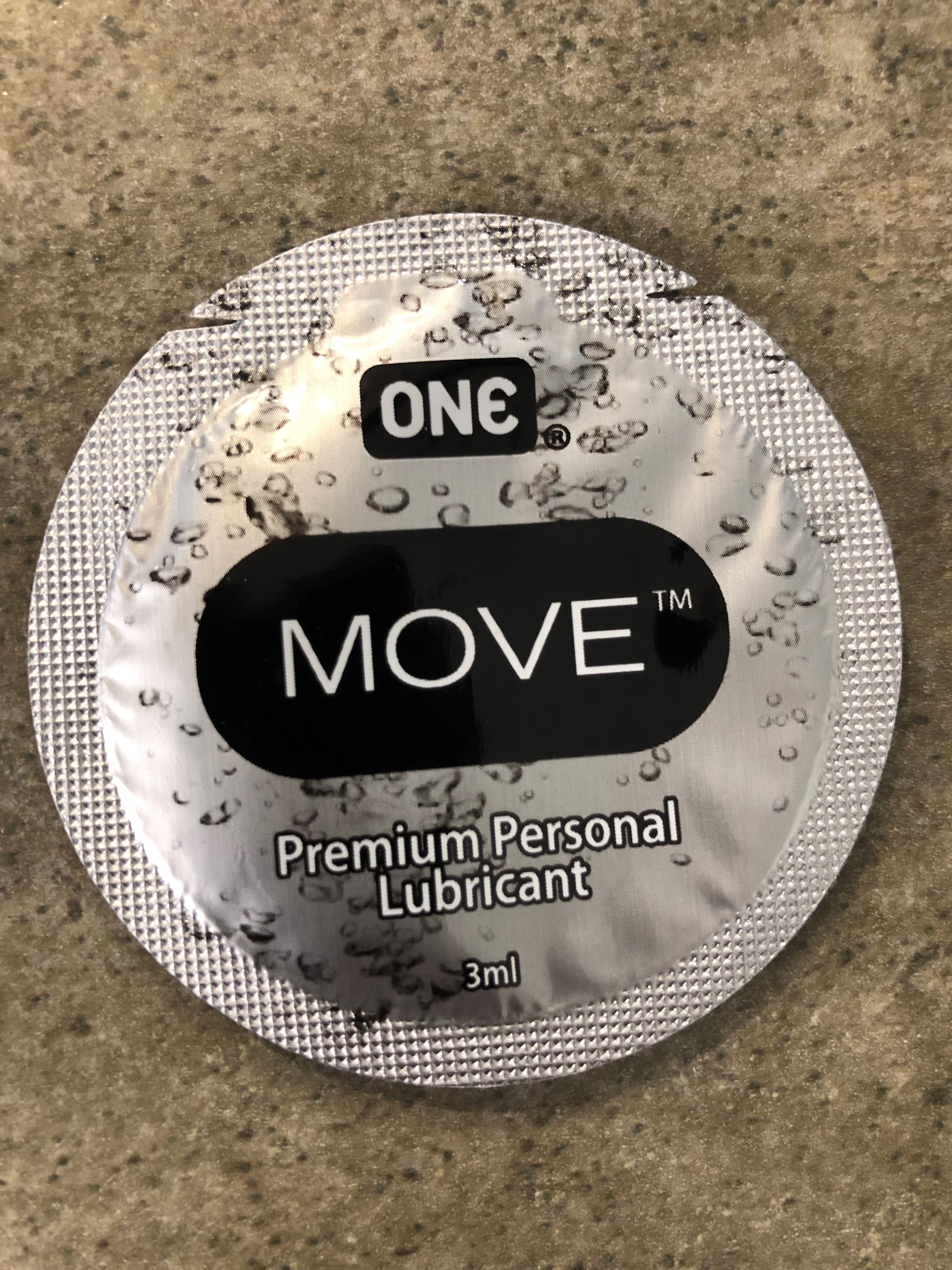  
Lubricants, Male and Female Condoms |
PWID engage in persistently high-risk behaviors, including unprotected sex, anal sex, and sex with more than one partner. The role of condoms as a protective prophylactic device is one of the most important safeguards against the spread of sexually transmitted diseases and HIV/AIDS. |
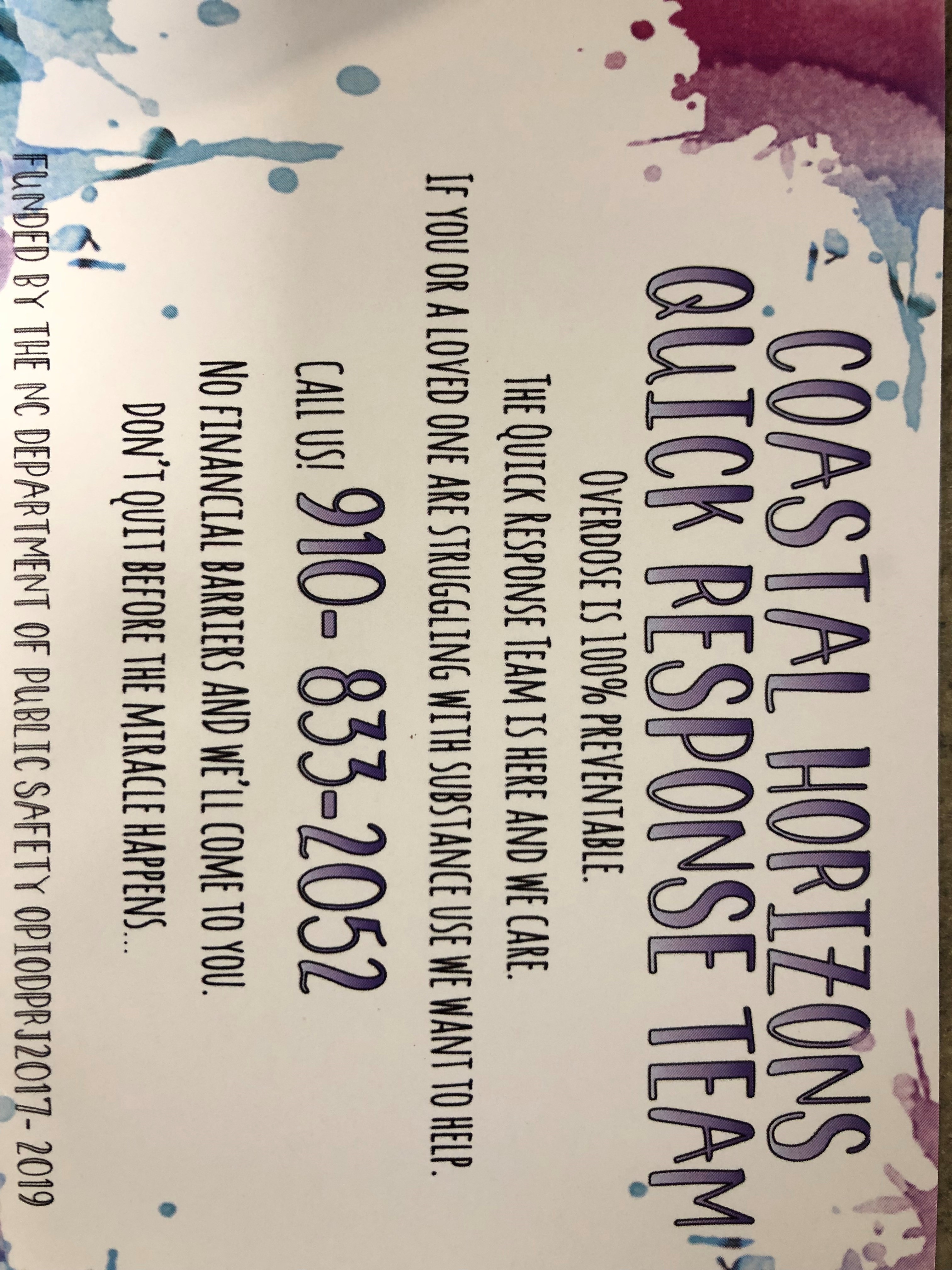
| Learn what resources SSPs make available to their clients |
Explore with the SSP which resources would be reasonable for the pharmacy to provide as an extension site and which ones might require referral back to the SSP.
For instance, education materials can easily be co-distributed at both locations; however, patients needing HIV, HCV, or STD testing or treatment may need referral back to the SSP.
|
|
Educational materials on overdose prevention, responding to an overdose, disease prevention, and treatment options (MOUD)
|
|
|
|
On-site MOUD or PrEP
Some SSPs are currently piloting these services.
While pharmacies do not currently have provisions for providing PrEP, they can provide PEP for those in need of post-exposure HIV prophylaxis
(See NCAP's PEP Toolkit and Training for more details)
Partnering with MOUD providers in managing patients in treatment for SUD is also a rapidly expanding practice among pharmacists.
(See Harm Reduction Toolkit- MOUD for more details)
|
Hormonal Contraception
Pharmacists can now assist SSPs in providing clients hormonal contraception if needed
(See NCAP's Hormonal Contraceptive Training and Toolkit for more details) |
Immunizations
Pharmacists are the largest providers of immunizations to the population at-large and can assist SSPs in delivering necessary immunizations to clients. |
|
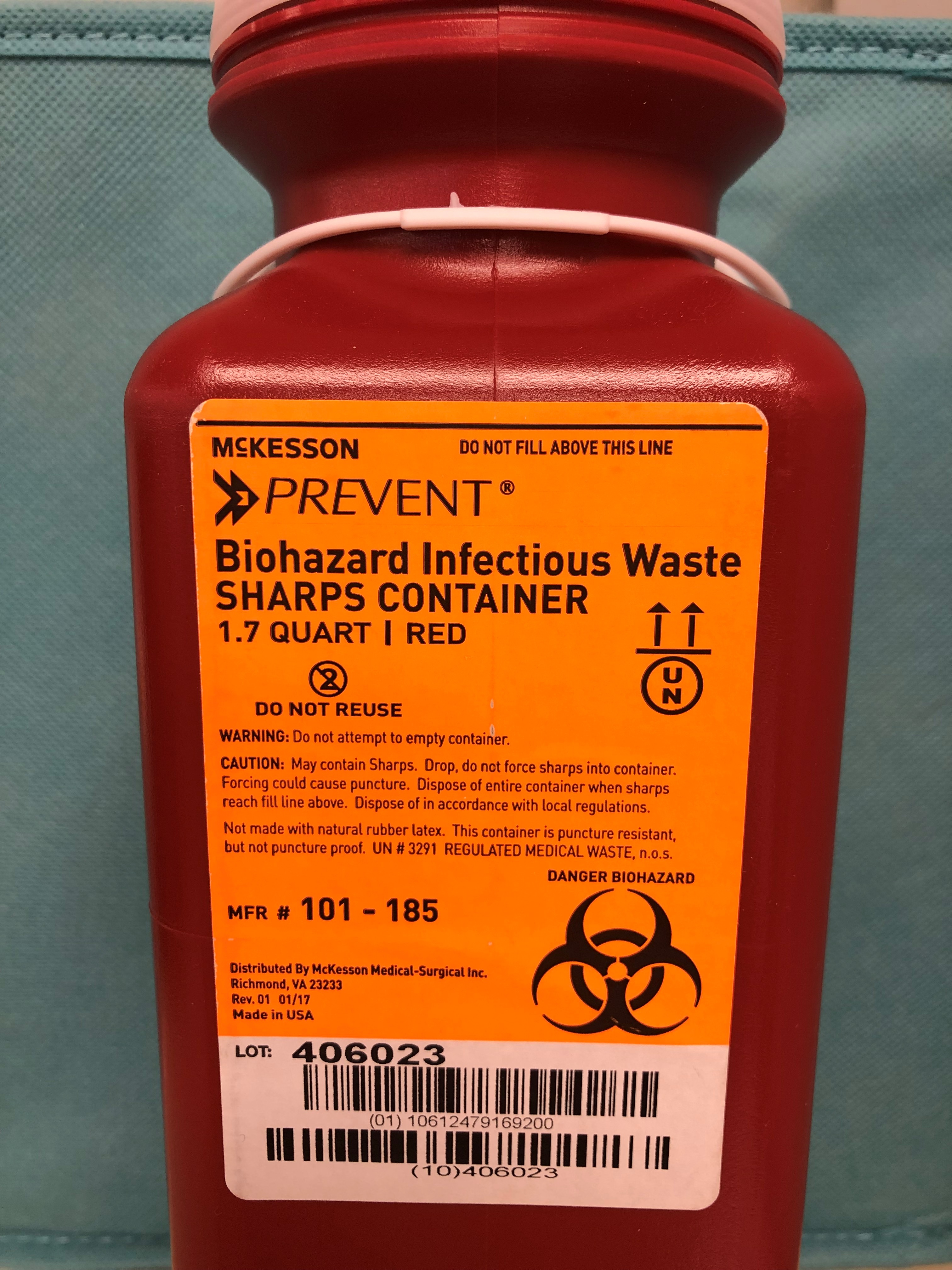
Syringe Disposal
SSP clients are encouraged but not required to return used syringes and supplies even though NC SSPs are required to have a means for disposal of these biohazardous materials. If a patient does return used supplies, the SSP must capture the number of returns for annual reporting to the Department of Public Health (DPH). Many pharmacies do not have the capacity or financial means to appropriately handle or dispose of biohazardous wastes. You will want to include this in your discussion with the SSP to determine how best to carry out this service.
In NCAP's Pilot, the Pharmacy sites openly accepted the return of used supplies. Per the Pharmacy's written Policy and Procedures, clients were provided sharps containers in their supply packets. Upon return, clients were asked to disclose the number of syringes returned at each visit, at which time the pharmacy staff would record the information on the client's syringe exchange log. Client returns were disposed of at the pharmacy as they already have biohazardous waste disposal due to their immunization program. At no time did staff touch or handle used needles or other injection equipment belonging to the client.
Sample Policy and Procedure
|
|
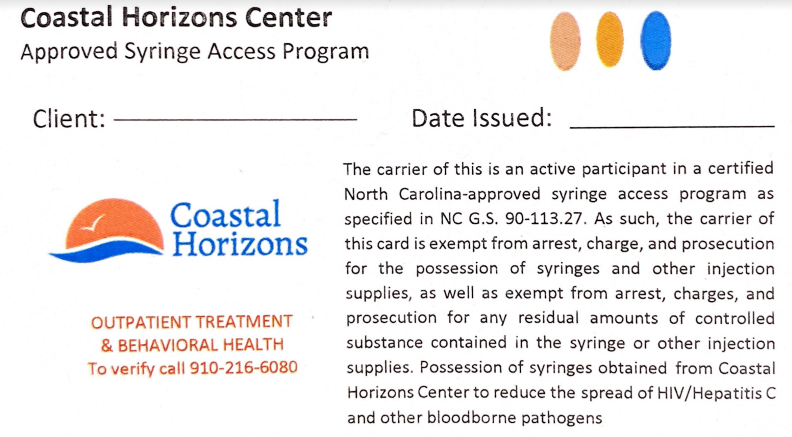
Participant Cards
"Limited Immunity Laws"
Syringe laws protect SSPs and clients from being charged with possessing syringes and injection supplies, including those with residual amounts of controlled substances.
Possession of Syringes/Tell Law Officer Law (G.S. 90-113.22)
Syringe Exchange Law (G.S. 90-113.27)
SSPs must provide clients with a written 'participant card' to verify their participation and be granted limited immunity during an arrest. DPH also encourages SSPs to share these participant cards with local law enforcement to demonstrate a client's involvement in the program and the entitlement to immunity for possessing syringes and other injection supplies.
In NCAP's Pilot, the participating pharmacies kept a supply of participant cards if they were the enrolling site for a new client.
|
| Consider Discussing With the SSP a Co-Location Process for Referring Clients |
|
Referal from the SSP to the Pharmacy
How will SSPs inform clients of their pharmacy extension site?
How will Pharmacies ID existing SSP clients for supply exchange?
|
Referral from the Pharmacy to the SSP
How will pharmacies go about enrolling NEW SSP clients?
|
|
SSPs participating in NCAP’s Pilot initiative developed a brochure to advertise their pharmacy extenders' names and contact information. See the example below.
During a visit, the SSP staff member would check the participant's county of residence, and if they resided closer to the pharmacy, they were personally handed the brochure to highlight the new, more convenient location.

(Click image to enlarge)
|
With the maturity and growth of your collaboration, a pharmacy will encounter patients in need of services. Still, they are not linked with your partnering SSP. It's important to discuss with the SSP how you will enroll and process new clients and how to communicate new client information back to the SSP.
NCAP's Pharmacy Pilot sites followed the new enrollee workflow below and used an exchange log to capture new enrollee information and distribution of supply kits. Pharmacists would assign the client a member ID#, issue a participant card, and initial confirmation that the client received a supply kit.
See workflow and exchange log below
(Click image to enlarge)
|
|
As an SSP extension site, pharmacies will co-manage clients already enrolled with their partnering SSP. It's important to discuss with the SSP how the pharmacy will identify existing clients before distributing supplies.
NCAP's Pharmacy Pilot sites simply confirmed a patient's enrollment in the SSP by verifying the client's SSP participant card.
See workflow below
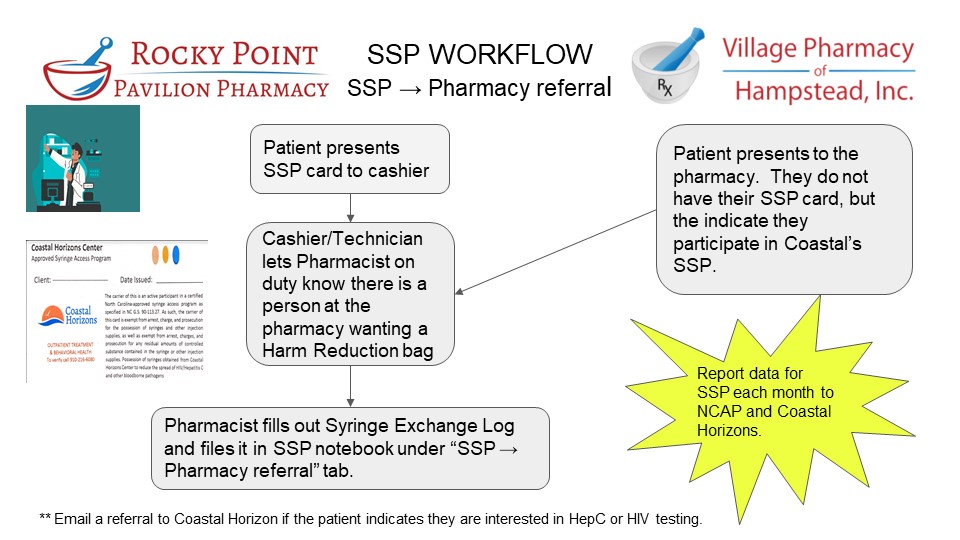 (Click image to enlarge) (Click image to enlarge)
|
In NC, DPH requires all SSPs to submit annual reporting to monitor program development and service coverage. The number of enrolled clients and supplies distributed and returned comprise that yearly report.
Best practices from NCAP's Pilot resulted in pharmacies using the exchange log to capture supply returns. Pharmacists would pull the log upon a client's return and use it to record the client's self-report of returned contents. Used supplies were destroyed at the pharmacy given they already had the means to destroy biohazardous materials through their immunization program. The log was housed at the pharmacy until the SSP could retrieve it for recordkeeping.
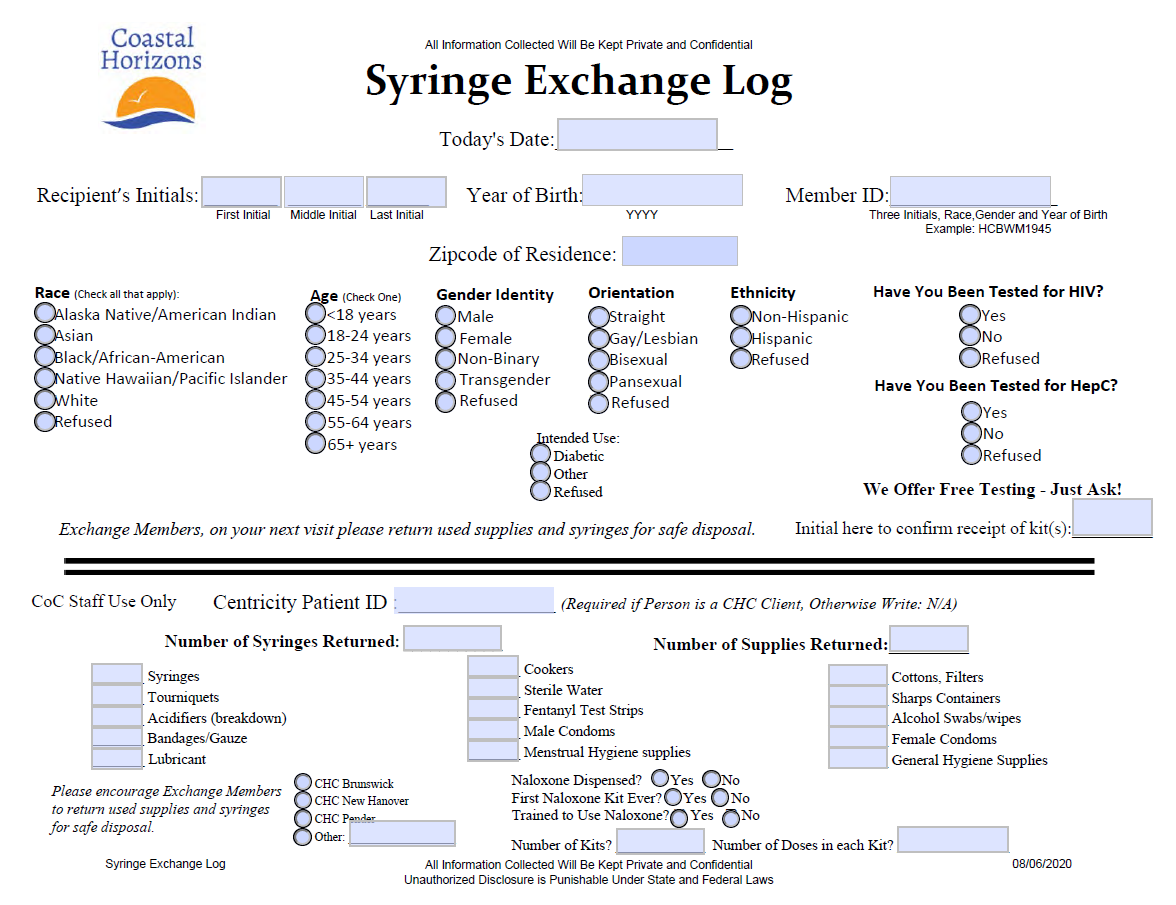
(Click image to enlarge)
|
Understand the SSPs Security Plan
|
| All SSPs in NC are required to submit a security plan to local law enforcement agencies to help ensure they are aware of the program and are familiar with the limited immunity provision |
| An SSP is considered "active" in a given county once the security plan is distributed to appropriate law enforcement |
| SSPs must review, make any changes as needed, and redistribute plans annually to law enforcement |
| In NCAP's Pilot, the participating pharmacies in Pender County partnered with an SSP in Brunswick and New Hanover Counties. The SSP had an established relationship and shared security plan in place with local law enforcement in Brunswick and New Hanover; however, with the addition of the Pender County pharmacies, it was necessary to update the plan with the new locations and further ensure support by sharing the new plan with Pender County law enforcement. This was easily accomplished through a phone call with the Pender County Sheriff's Department. |
|
Sample SSP Security Plan
|
|
Additional Information and Quick Answers to Share With Law Enforcement
|
Work With the SSP to Develop a Plan for 'Spreading the Word'
About the New SPP Pharmacy Sites |
| Recognize that uptick in new clients is likely to be a slow and gradual process. It will take time to build awareness in the community, especially if you reside in a desert area with little to no community harm reduction resources. Advertising in concert with broader education will likely be needed to create a positive shift in attitude and engagement in the community. |
| Ideas cultivated for NCAP's Pilot initiative are listed below |
Create Brochures/Flyers (See above) in Spanish and English if possible
Both Pharmacies and SSPs should share with their patrons to promote services in their respective locations |
Share Brochures/Flyers With Local Health Departments (HD).
Find out if the HD provides any Substance Use Disorder (SUD) ancillary services within their clinics. If so, ask for a contact to establish the best person for distributing the materials to patients in need. |
Share Brochures/Flyers With Local Law Enforcement.
Foster relationships by offering to provide education/training on Harm Reduction practices and SSP services to law enforcement personnel |
| Share Brochures/Flyers With First Responders |
| Share Brochures/Flyers With Local Food Banks |
| Share Brochures/Flyers With Hospitals (ED Departments or Outpatient Pharmacy) |
| Provide Brochures/Flyers During National or Local Drug Take Back Events |
| Share Brochures/Flyers With Local Vape Shops and CBD Stores |
Check Community Event Calendars
Consider participating in community events where you can distribute brochures and educational materials to strengthen community awareness |
| Become a Community Stakeholder and Get Connected |
| Work with the SSP in connecting to local/state tasks forces, coalitions, and other groups that can help support your SSP efforts |
| |
Option 3
Start Your OWN Syringe Service Program |
|
According to NC law,
“any governmental or nongovernmental organization that promotes scientifically proven ways of mitigating health risks associated with drug use and other high-risk behaviors can start a syringe services program.”
This includes Pharmacies
|
|
For information on how you can start your own SSP Service visit
The North Carolina Safer Syringe Initiative
OR email
[email protected]
|